|
What you need to know about
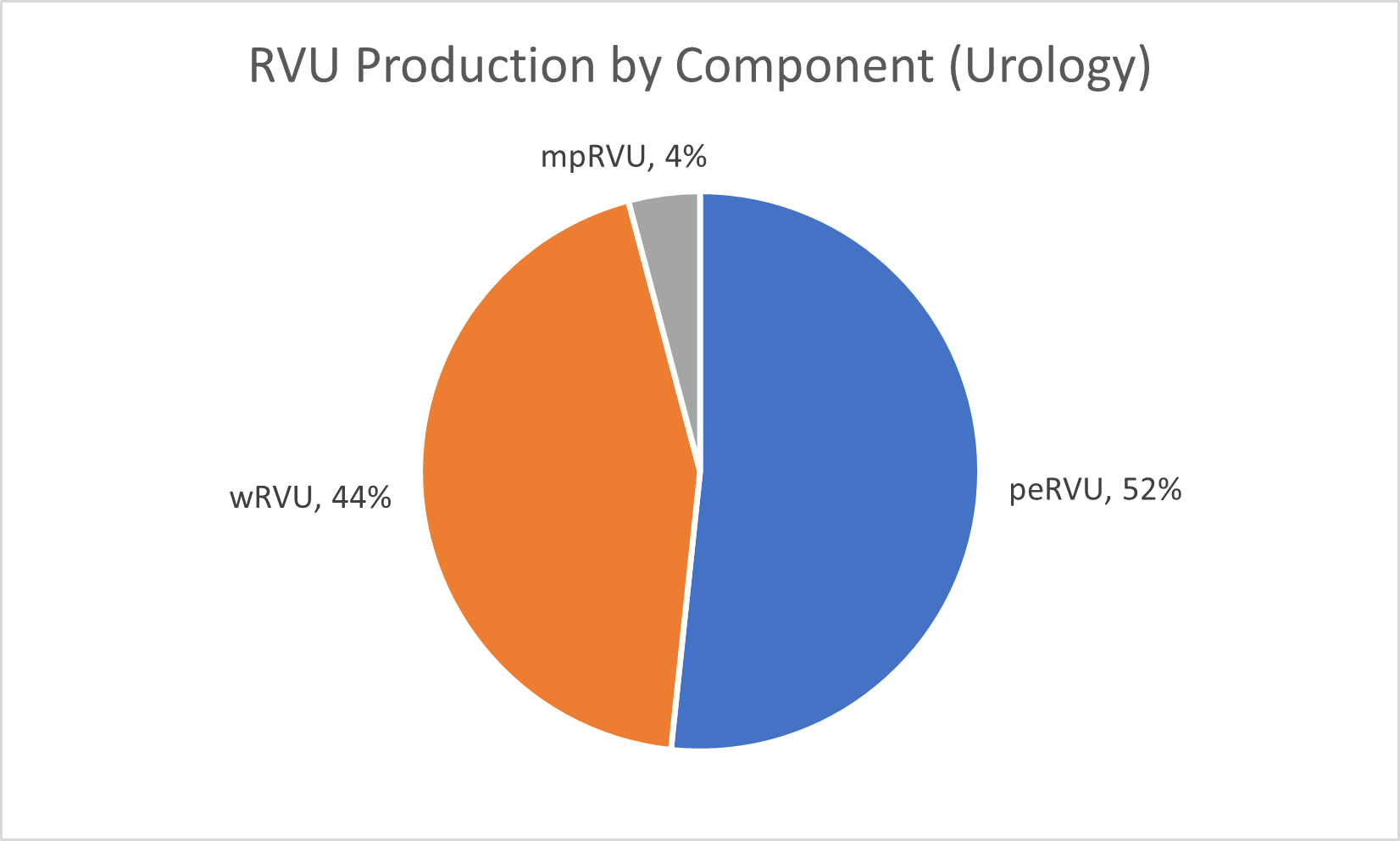
Dec. 2021 RVU Basics RVUs are a part of the resource-based relative value scale (RBRVS) used to calculate the Medicare reimbursement for physician services. They represent a standardized method for valuing the amount of physician work, clinical and nonclinical practice resources, and expertise required to service patients. Relative Value Units (RVU) Components
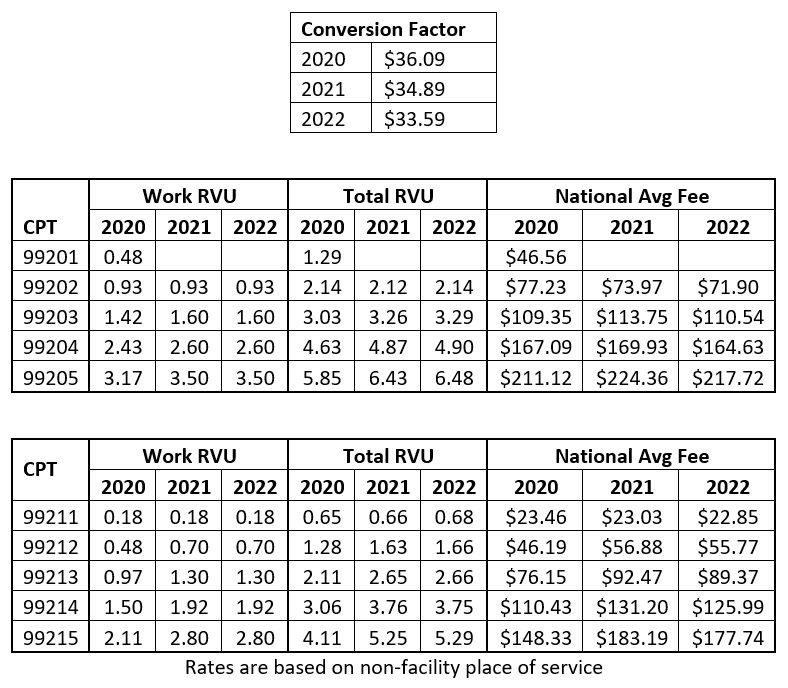
Payment for services is calculated by applying a Geographic Practice Cost Index (GPCI) to each RVU component and multiplying by the conversion factor which in 2021 is $34.89. The GPCI adjusters raise or lower each component to account for geographic differences in physician costs, practice staffing and operations, and malpractice insurance. Medicare Allowable Pricing Formula [(Work RVU * Work GPCI) + (PE RVU * PE GPCI) + (MP RVU * MP GPCI)] * Conversion Factor
Trends in RVUs The 2021 PFS significantly increased the RVU value for several Evaluation and Management (E/M) CPT codes, which account for 54% of work RVU production for urologists. To comply with budget neutrality, there was a corresponding decrease in the conversion factor. The reduced conversion factor is applied to all physician services which resulted in decreases to many of the surgery, radiology, and physical therapy CPTs, offsetting any increases from the RVU changes to E/Ms.
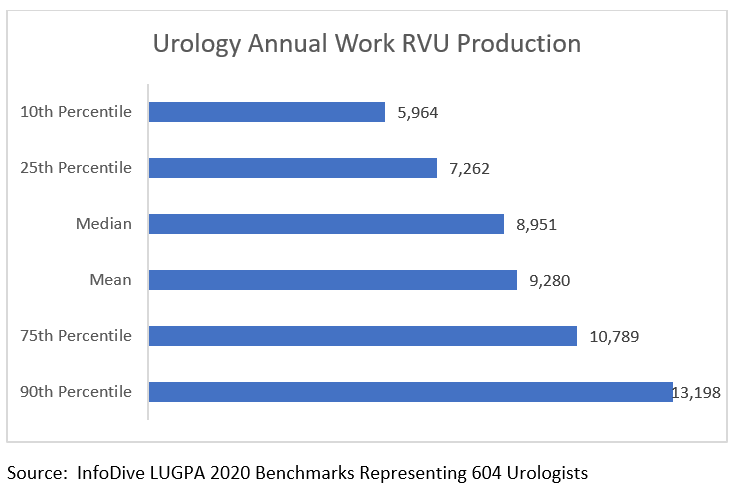
wRVUs and Compensation The use of wRVUs is considered a more equitable method to measure provider productivity as each service is valued based on the time and skill involved to deliver the service. Patient visits, surgical cases and days worked do not to accurately measure production. Use of revenue as a measurement is skewed by a provider’s payer mix. For example, a provider who performs a high volume of vasectomies would have a greater portion of revenue from self-pay and commercial plans, which typically pay at higher rates than Medicare, than those treating more senior patient populations. Work RVU’s continue to be the most frequently utilized volume-based production incentive and were featured in 59% of Merritt Hawkins’ recruiting assignments in which a production bonus was part of the incentive package, up from 57% last year1. Challenges Senior leadership is responsible for ensuring physicians understand how RVUs are calculated including nuances such as adjustments for multiple procedures, bilateral, and assistant surgeries. There should be clear understanding of how to account for work that cannot be measured by RVUs such as unlisted surgical codes that have yet to be assigned an CPT and call duty. When wRVUs increase more than reimbursement, physician compensation growth can outpace reimbursement growth and negatively impact margins. Do you know the impact to your practice? Practices must create a financial strategy that allows them to account for necessary compensation increases while dealing with a dormant or decreasing level of reimbursement because of RVU and conversion factor changes. A growing percentage of physician employment contracts factor wRVU production into the compensation plan, especially with the increased volume of providers associated to health systems and private equity organizations. Often there are minimum thresholds built into the compensation plan. Listed below examples of median values of annual wRVUs production:
RVUs are the most used concept in medical practice management. They provide a common framework in which to construct payer contract rates, assess operational costs and measure provider productivity. Whether your practice uses wRVUs in your compensation plans today, there is much value to tracking and sharing wRVU production with your providers.
|